Digital Clinic - BMPR2 case study
Miss Charlotte Smith, BMPR2 case study - last updated 07 May 2025

Miss Smith is a 21-year-old lady, who has become progressively breathless over 2 years. Her general practitioner has been treating her for asthma with increasing inhaled therapy, but she is not improving.
The symptoms of pulmonary hypertension arise primarily from right ventricular dysfunction and right ventricular failure. The commonest symptom is shortness of breath on exertion. Other symptoms include fatigue, exertional dizziness, collapse or chest pain, palpitations and ankle swelling. Cough is often a feature suggesting significant pulmonary arterial or right atrial enlargement. The mechanism is believed to be compression of a bronchus by the enlarging vessel/atrium.
Stage 1: Initial consultation at a general clinic
This patient has symptoms of progressive exertional breathlessness. There have been some pre-syncopal symptoms, but no defined collapses. She does have a cough, which can be a symptom of pulmonary hypertension. Empirical treatment for asthma has not really helped. There is an interesting family history of pulmonary hypertension which could be a strong predisposing risk factor in this patient.
There is a loud P2 and a murmur consistent with tricuspid regurgitation which would suggest the presence of PH. She also has some mild features to suggest a degree of right ventricular dysfunction with an elevated Jugular venous pressure and some peripheral oedema.
The signs due to pulmonary hypertension are subtle and include right ventricular heave, loud split P2, a right third or fourth heart sound and an early diastolic murmur due to pulmonary regurgitation. Signs due to right ventricular failure are more easily discerned such as an elevated JVP, pansystolic murmur of tricuspid regurgitation, peripheral oedema and ascites. Auscultation of the lungs is usually normal. There may also be signs of an underlying condition predisposing to pulmonary hypertension.
General
- Slightly overweight lady with a BMI of 29kg/m2
- No clubbing
- No signs of connective tissue diseases (no rash, sclerodactyly, calcinosis)
Cardiovascular
- Heart reate 82 bpm in sinus rhythm
- Blood pressure 127/72 mmHg
- JVP was raised to 4cm and there is mild ankle oedema
- There was a loud P2 and a quiet PSM left sternal edge, louder on inspiration
Respiratory
- Chest was clear to auscultation and in particular there was no wheeze
Abdomen
- Normal
Stage 2: Specialist pulmonary hypertension centre
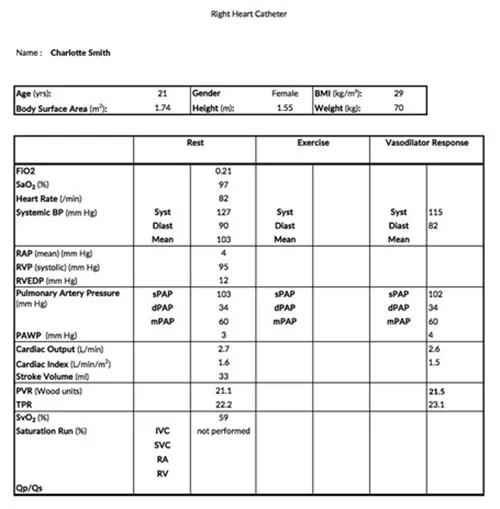
Further tests were performed at a specialist centre by a multi-disciplinary team.
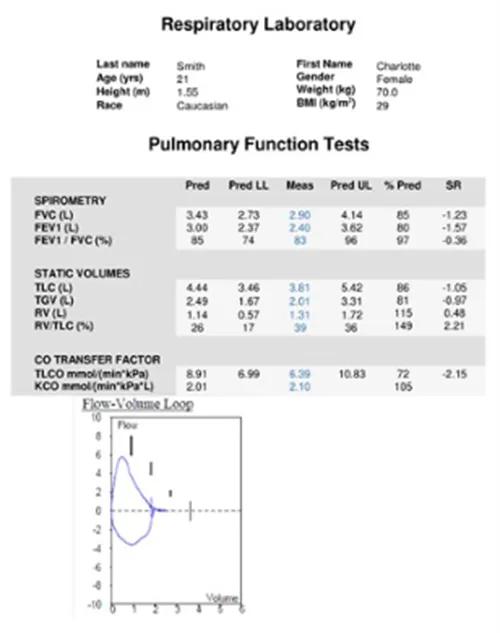
This test result shows signs of abnormality. The lung volumes are within normal limits. There is an isolated low transfer factor. This pattern would be consistent with PAH.
The role of pulmonary function tests in pulmonary hypertension is to identify airway or parenchymal lung disease. In pulmonary arterial hypertension (PAH) there may be mild to moderate reduction in lung volumes and occasionally mild airflow obstruction, particularly at the peripheral level. Most people with PAH have decreased transfer factor.

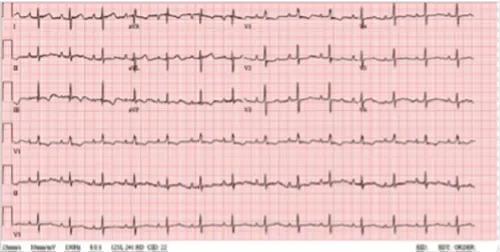
There is right axis deviation, with some inferior and anterior T wave changes. There is borderline right bundle branch appearance. Non-specific ST segment change in V1-2.
The ECG is often but not always abnormal in pulmonary arterial hypertension. The most sensitive feature is RV strain (ST depression and T wave inversion in leads V1 to V3). Other changes found include right axis deviation, P pulmonale, right bundle branch block, tall R waves especially anteriorly and prolonged QTc.
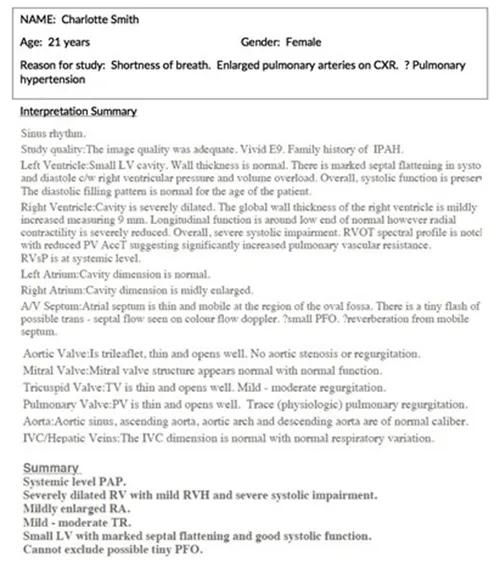
The echocardiogram is probably the most important non-invasive test in the diagnosis of pulmonary hypertension as it will often be the investigation which will decide on further diagnostic tests for the patient. It is important to remember that although this is an important test it is not the gold standard diagnostic test for PAH. That remains the right heart catheterisation. The important measurements in the echo focus on the pulmonary artery pressure (measured by tricuspid regurgitant velocity or pressure gradient) and the RV morphology. Key parameters include the RV dimensions and RV function.
Occasionally the TRV cannot be accurately measured and in these circumstances other parameters which may indicate PAH should be assessed. These include RV morphology and pulmonary artery acceleration time. In addition echo parameters such as Tricuspid annular planar systolic excursion(TAPSE) can be used to aid in patient prognosis. Echo can also be used to assess the underlying cause of the pulmonary hypertension. For example an enlarged LA can indicate heart failure with preserved ejection fraction and an assessment of valvular function can indicate mitral regurgitation or aortic stenosis. In patients with hypoxaemia, an assessment using agitated saline should be made to investigate the presence of a significant right to left intracardiac shunt.

The radiologist report is as follows "PA projection. Cardiothoracic ratio is 135/265. Heart size is at upper limit of normal. There is central pulmonary vascular prominence. Lungs are clear.”
The chest x-ray is abnormal in 90% of people with idiopathic pulmonary arterial hypertension (IPAH) at the time of diagnosis. Typical changes include enlarged pulmonary arteries with peripheral pruning of vessels and cardiomegaly with a boot shaped heart. There may be changes suggesting an alternative cause of pulmonary hypertension such as lung disease or pulmonary venous congestion.
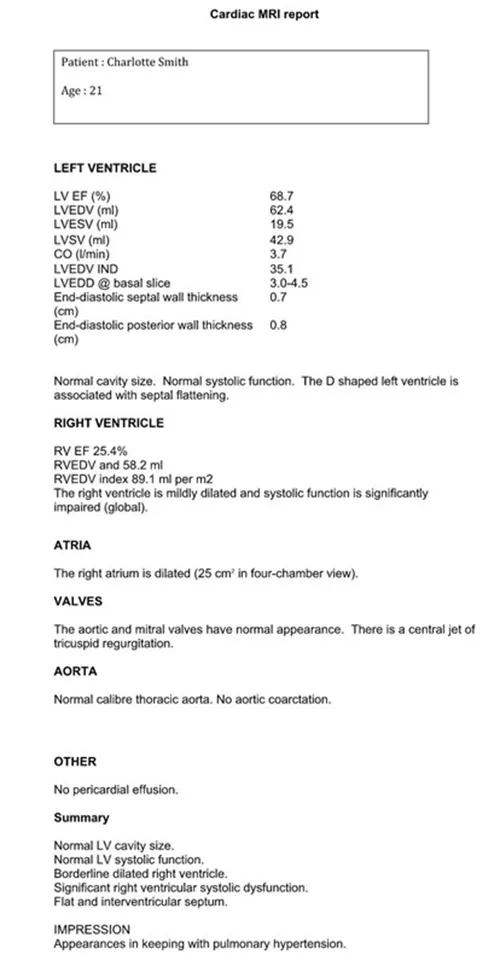
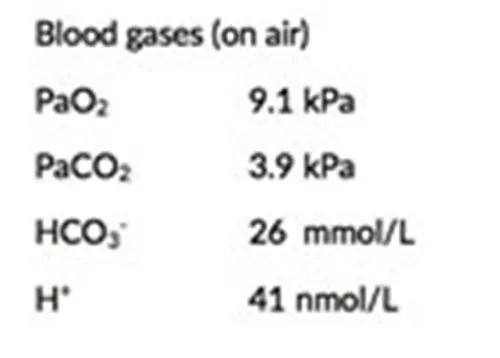
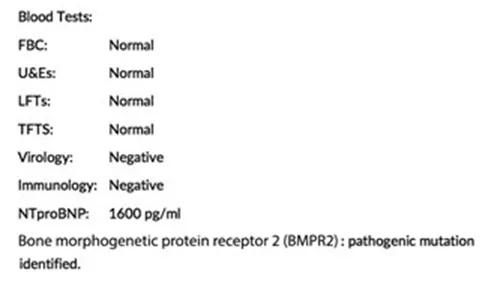
Miss Smith was diagnosed with Heritable PAH (BMPR2 Positive).
Risk of this patient dying within one year |
|||
| Risk factor | Low | Medium | High |
| Clinical signs of right heart failure | X | ||
| Progression of symptoms | X | ||
| Syncope | X | ||
| WHO functional class | X | ||
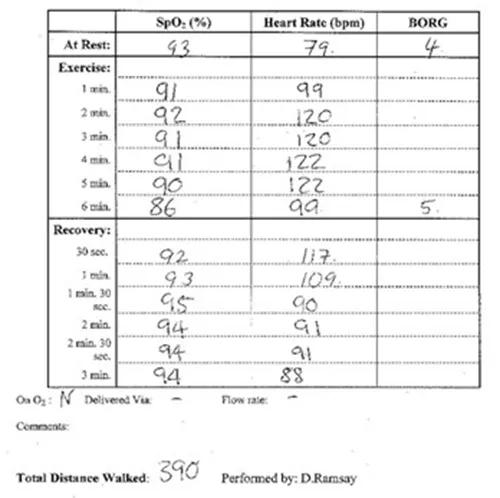
| 6MWD | X | ||
| Cardiopulmonary exercise testing | X | ||
| NT-proBNP plasma levels | X | ||
| Imaging (echo, CMR imaging) | X | ||
| Haemodynamics | X | ||
Stage 3: Treatment
• Phosphodiesterase Type 5 Inhibitors – Primary drug
• Endothelin Receptor Antagonists – Primary drug