Digital Clinic - Pregnancy case study
Mrs Yasmin Colins, pregnancy case study - last updated 07 May 2025

Mrs Colins is a 23-year-old woman who is 18 weeks into her first pregnancy and has been referred to a cardiologist after presenting to the ER following an episode of collapse with loss of consciousness.
Examination is a key part of the initial assessment. It also aids assessment of disease severity and can give clues to the aetiology. It should be appreciated that clinical signs of pulmonary hypertension can be very subtle and are normally best appreciated once the diagnosis is known.
Stage 1: Initial consultation at a general clinic
This patient has a history of exertional shortness of breath and recurrent exertional syncope. This would fit with a diagnosis of pulmonary arterial hypertension.
In the assessment of a patient with suspected pulmonary hypertension, the history is key in helping to identify the likelihood of pulmonary hypertension, establishing disease severity and clues to the aetiology of disease. It should include a careful cardiorespiratory history. Blackouts are often a marker of disease severity. When they occur on minimal exertion, they reflect poor right ventricular function. Blackouts, however, may also occur particularly in younger patients with idiopathic pulmonary arterial hypertension (IPAH) on more strenuous exertion and are not uncommon in patients with idiopathic pulmonary arterial hypertension who are vasodilator responders. In young patients, ankle swelling is very uncommon and if present usually reflects severe disease. A comprehensive assessment of risk factors for pulmonary hypertension is key to aid accurate classification of disease. This patient had no risk factors for pulmonary hypertension. The social history is very important, in particular to identify support networks for the patient. Where patients live in a chaotic social environment, extra care must be taken to ensure that they are well supported.
General
- Looks well, BMI 23, oxygen saturation 98% in hands and feet
- No scleroderma, no telangiectasia, no dilated nail fold capillaries
- No finger clubbing
Cardiovascular
- P 96 bpm regular BP 124/72 JVP seen in the route of the neck
- Loud P2 and pan-systolic murmur
- No ankle oedema
Respiratory
- Vesicular breath sounds with good air entry and no added sounds
Abdomen
- Pregnant consistent with 18 weeks
On examination, this patient has a loud P2 and a pansystolic murmur, one cause of which is tricuspid regurgitation. These are both features of pulmonary hypertension.
In idiopathic pulmonary arterial hypertension, resting hypoxaemia is very rare in the absence of severe disease. In pre-capillary pulmonary hypertension hypoxaemia usually suggests a problem with gas exchange e.g. due to coexisting lung disease or in systemic sclerosis where gas transfer is often impaired even in the absence of interstitial lung disease) or hypoventilation in patients with obesity hypoventilation syndrome. It may also be seen in patients with right to left shunts. In patients with a patent ductus arteriosus, oxygen saturation may be well maintained in the hands (and no clubbing) but there may be significantly lower saturations in the feet (which may be clubbed) due to the site of the right to left shunt.
The cardiologist decided to refer Mrs Colins to a specialist pulmonary hypertension centre.
Stage 2: Specialist pulmonary hypertension centre
Further tests were performed at a specialist centre by a multi-disciplinary team.
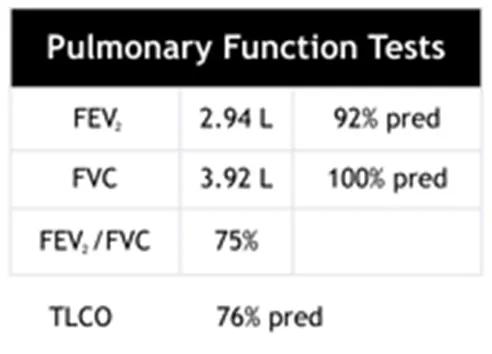
There are normal lung volumes and a mildly reduced TLCO, which is compatible with a diagnosis of pulmonary arterial hypertension.
Spirometry and gas transfer assessment are key measurements. They may suggest an alternative cause for symptoms of breathlessness in addition to aiding classification of disease. Performing spirometry alone is not sufficient to exclude respiratory disease as a significant proportion of patients with normal spirometry and pulmonary hypertension will have underlying lung disease. It would be uncommon, however, to have respiratory disease sufficient to cause pulmonary hypertension and normal gas transfer. In the setting of pulmonary hypertension a severe reduction in gas transfer (TLCO) less than 50% should raise the possibility of co-existing lung disease or systemic sclerosis. In idiopathic pulmonary arterial hypertension a lower gas transfer usually reflects more severe disease. In the setting of pulmonary hypertension a normal or increased TLCO should raise the possibility of a left to right shunt.
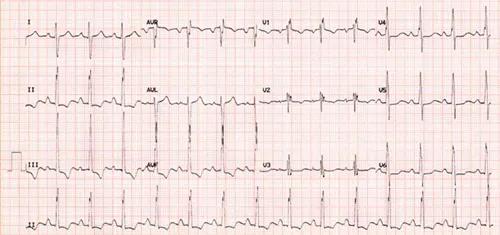
The ECG shows right axis deviation and ST depression in the inferior leads which are both consistent with pulmonary hypertension.
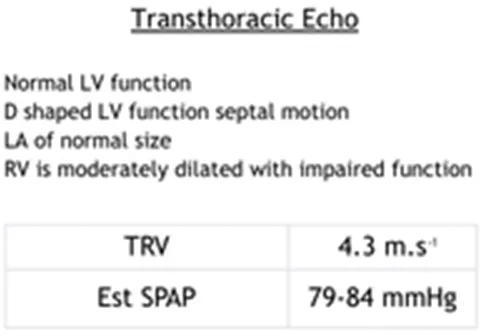
The transthoracic echo shows a TRPG of 74 mmHg with a dilated right heart with impaired function and a normal left heart. There is no evidence of intracardiac shunt. The LV is D-shaped and there is paradoxical septal motion. These are typical features seen in pulmonary arterial hypertension.
Echocardiography is recommended as the first non-invasive imaging test when pulmonary hypertension is suspected. The echocardiographic assessment includes an estimate of systolic pulmonary artery pressure and an assessment for other features of pulmonary hypertension. The echocardiogram may suggest a cardiac cause including valvular heart disease or left ventricular systolic or diastolic dysfunction. Features highly suggestive of precapillary pulmonary hypertension include the presence of paradoxical septal motion, and significant impairment of right ventricular function.
Assessment of left atrial size is also very important. An enlarged left atrium should ensure that a detailed assessment is undertaken to exclude left heart disease such as heart failure with preserved ejection fraction. The presence of systolic pressure greater than 70mmHg with an enlarged left atrium and the absence of paradoxical motion (suggesting with this level of sPAP that left sided pressures are elevated) is highly suggestive that left heart disease is the cause although systematic assessment is still required to exclude other co-existing causes.

The chest x-ray shows a degree of pulmonary artery enlargement, which would suggest pulmonary hypertension.
In patients with pulmonary hypertension the CXR is often abnormal. However, it may be normal particularly in patients with less severe pulmonary hypertension. Pulmonary artery enlargement is usually better appreciated on CT imaging.
How convinced are you that this patient has pulmonary hypertension based on this chest x-ray?
Feedback from the multi-disciplinary team
Mrs Colins was diagnosed with idiopathic pulmonary arterial hypertension (vasodilator responder).
Risk of this patient dying within one year |
|||
| Risk factor | Low | Medium | High |
| Clinical signs of right heart failure | X | ||
| Progression of symptoms | X | ||
| Syncope | X | ||
| WHO functional class | X | ||
| 6MWD | |||
| Cardiopulmonary exercise testing | |||
| NT-proBNP plasma levels | |||
| Imaging (echo, CMR imaging) | X | ||
| Haemodynamics | X | ||
In pregnant patients with suspected pulmonary hypertension, it is key that patients undergo systematic evaluation. Due to the high risk of maternal death, these patients should ideally be counselled and managed by centres with experience in the management of pulmonary hypertension in pregnancy.
Hemnes, AR, Kiely DG, Cockrill BG, Safdar Z, Wilson VJ, AI Hazmi M, Preston I, Maclean M, Lahm T. Statement on pregnancy in PH from the PVRI Pulmonary Circulation 2015;5(3)c435-65.
Bedard E, Dimopoulos K, Gatzoulis M, Has there been any progress made on pregnancy outcomes among women with pulmonary arterial hypertension. Eur Hear J 2009;30(3):256-65.
Kiely DG, Condliffe R, Wilson V, Gandhi S, Elliot CA. Pregnancy and pulmonary hypertension: a practical approach to management. Obstetric Medicin 2013;6(4):144-154.
Jais X, Olsson KM, Barbera JA, Blanco I, Torbicki A, PEacock A, Vizza CD, Macdonald P, Humbert M, Hoeper MM. Pregnancy outcomes in pulmonary arternail hypertension in the modern management era. Eur Respir J. 2012 Oct;40(4):881-5.
Kiely DG. Condliffe R. Webster V, Mills GH, Wrench I, Gandhi SV, Selby K, Armstrong IJ, Martin L., Howarth ES, Bu'lock FA, Steward P, Elliot CA. Improved survival in pregnancy and pulmonary hhypertension using a mutiprofessional approach. BJOG. 2010 Apr;117(5):565-74.
Elliott CA, Stewart P, Webster VJ, Mills GH, Hutchinson SP, Howarth ES, Bu'lock FA, Lawson RA, Armstrong IJ, Kiely DG. The use of iloprost in early pregnancy in patients with pulmonary arterial hypertension. Eur Respir J.2005 Jul;26(1):168-73.
Stage 3: Treatment
Case study summary
In this case, following counselling by an experienced multi-professional team, the patient elected to undergo a late medical termination. This was performed in a critical care setting with central and arterial access and monitoring of central venous pressures, central oxygen saturations and non-invasive continuous monitoring of cardiac output using LiDco.
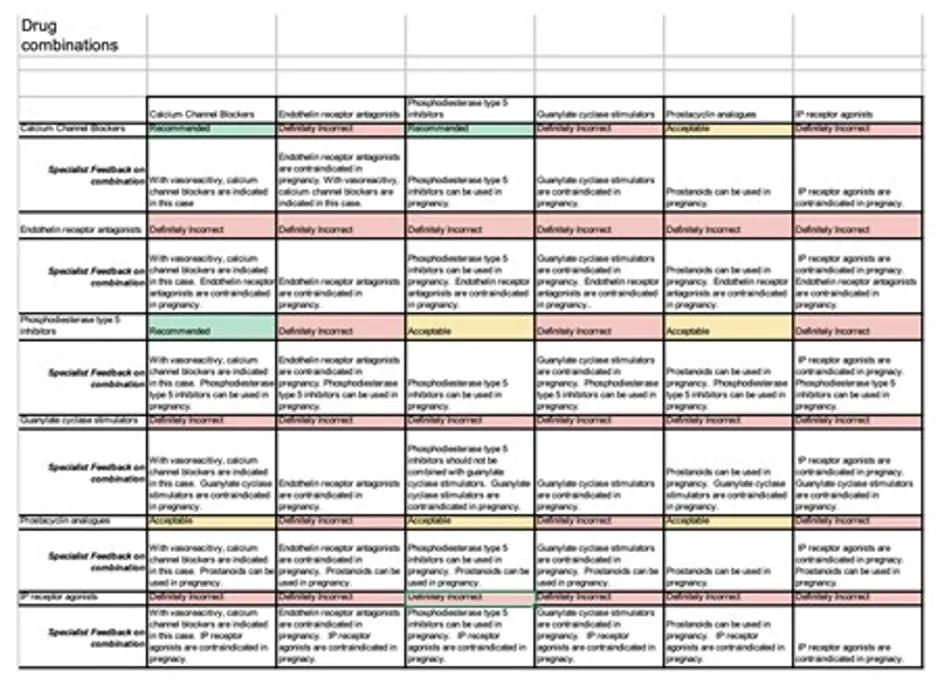
The patient was commenced on calcium channel blockade with Slozem XL (Diltiazem) 180 mg in addition to prophylactic doses of LMWH and nebulised iloprost (5mcg) x 6 /day). The aim was to uptitrate to a maximal tolerated dose of Slozem XL and withdraw nebulised iloprost at 3 months depending on satisfactory progress. Following further discussion regarding the risks of pregnancy and pulmonary hypertension the patient elected to have a hormonal implant (Nexplanon) which was inserted prior to discharge.
The patient was discharged 72 hours following termination. The patient has made excellent progress and at 18 months following the diagnosis she is in a low risk group based on ESC/ERS guidelines being in WHO FC I with a normal exercise capacity (ISWT 93% predicted) and having a normal NT-proBNP. Her follow-up cardiac MRI at one year following diagnosis shows normal right ventricular volumes and function with a RVEF of 55%.
She continues to work full-time. Given her desire to have a family further discussions have taken place with obstetric and the reproductive care team and members of the pulmonary hypertension team. Following counselling regarding the risks of pregnancy and discussing other options, such as adoption and surrogacy, the patient and her partner expressed a wish to pursue surrogacy as an option. The patient has now undergone ovarian stimulation with successful egg collection and embryo culture. The patient does not carry a mutation in a gene associated with pulmonary arterial hypertension but if present there is the option to screen embryos prior to implantation in a donor.
Patients with suspected pulmonary hypertension require systematic evaluation. Treatment depends on the underlying cause, but a presentation during pregnancy with previously undiagnosed pulmonary hypertension poses particular challenges.
Patients require a systematic evaluation and ideally should be seen in centres with experience managing patients with pulmonary hypertension in pregnancy.
The needs of the patient are paramount and they and their families must be supported to make informed decisions. This requires expert counselling by a multi-professional team. It is essential that whatever decisions are made that patients continue to receive support and tailored treatment.