Digital Clinic - Sclerosis case study
Mr Robert Brown, Sclerosis case study - last updated 07 May 2025

Mr Brown is a 63-year-old man who regularly attends a rheumatology clinic with systemic sclerosis. He has just had his annual screening echo for Pulmonary Hypertension (PH).
The symptoms of pulmonary hypertension arise primarily from right ventricular dysfunction and right ventricular failure. The commonest symptom is shortness of breath on exertion. Other symptoms include fatigue, exertional dizziness, collapse or chest pain, palpitations and ankle swelling.
Stage 1: Initial consultation at a general clinic
Mr Brown's symptoms are not prominent and have potential explanations other than suggesting the presence of Pulmonary Arterial Hypertension (PAH). Further tests are performed to check for abnormalities before deciding whether it is appropriate to refer this patient to a specialist PH centre.
General
- Well-built man with a BMI of 26 kg/m2
- There were signs of Parkinson’s disease – bradykinesia and resting tremor
- There was obvious Raynaud’s phenomenon with finger changes but no telangiectasia
Cardiovascular
- Heart rate 61/min in sinus rhythm
- Blood pressure 121 / 65 mmHg
- JVP was not elevated and there was no ankle oedema
- Heart sounds were normal
Respiratory
- Normal auscultation of lung fields
Abdomen
- Normal
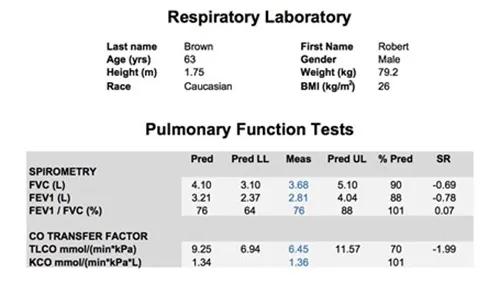
On spirometry this patient has normal lung volumes but disproportionately reduced transfer factor. These findings do not exclude PAH.
The role of pulmonary function tests in pulmonary hypertension is to identify airway or parenchymal lung disease. In pulmonary arterial hypertension (PAH) there may be mild to moderate reduction in lung volumes and occasionally mild airflow obstruction, particularly of the peripheral airways. Most people with PAH have decreased transfer factor.
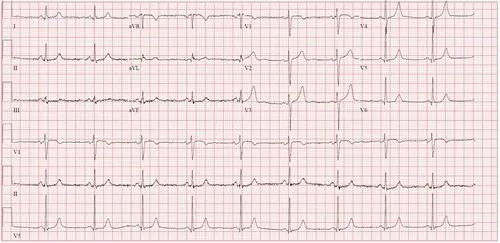
This ECG shows no abnormal features other than sinus bradycardia. It does not suggest PAH.
The ECG is often but not always abnormal in PAH. The most sensitive feature is RV strain (ST depression and T wave inversion in leads V1 to V3). Other changes found include right axis deviation, P pulmonale, right bundle branch block, tall R waves especially anteriorly and prolonged QTc.
Name: Robert Brown
- Age: 63 years
- Gender: Male
- Reason for study: Systemic sclerosis. Parkinson’s disease. ? pulmonary hypertension
Interpretation summary
- Sinus rhythm
- Study quality: Image quality was adequate
- Left ventricle: Non-dilated LV cavity. Wall thickness is normal. Overall systolic function is normal. Grade I diastolic dysfunction.
- Left atrium: Cavity dimension is normal (17 cm2).
- Right ventricle: Non-dilated RV cavity. Wall thickness is normal. The systolic function is normal. (TRV is 2.49 m/s and TRPG is 25 mmHg).
- Right atrium: Cavity dimension is normal (16 cm2).
- Aortic valve: Mild annular calcification. Trace of regurgitation.
- Mitral valve: Annular calcification and mildly thickened leaflets. Trace of regurgitation.
- Tricuspid valve: Normal. Mild regurgitation.
- Pulmonary valve: Thin and opens well.
- Pericardium: The pericardium is normal. No pericardial effusion.
The transthoracic echocardiogram in this patient shows a normal TRPG and normal right and left heart chambers. There are some minor abnormalities of the aortic and mitral valves.
The echocardiogram is probably the most important non-invasive test in the diagnosis of PH as it will often be the investigation which will decide on further diagnostic tests for the patient. It is important to remember that although this is an important test it is not the gold standard diagnostic test for PAH. That remains the right heart catheterisation. The important measurements in the echo focus on the pulmonary artery pressure (measured by tricuspid regurgitant velocity or pressure gradient) and the RV morphology. Key parameters include the RV dimensions and RV function.
Occasionally the TRV cannot be accurately measured and in these circumstances other parameters which may indicate PAH should be assessed. These include RV morphology and pulmonary artery acceleration time. In addition echo parameters such as Tricuspid annular planar systolic excursion(TAPSE) can be used to aid in patient prognosis. Echo can also be used to assess the underlying cause of the PH. For example an enlarged LA can indicate heart failure with preserved ejection fraction and an assessment of valvular function can indicate mitral regurgitation or aortic stenosis. In patients with hypoxaemia, an assessment using agitated saline should be made to investigate the presence of a significant right to left intracardiac shunt.
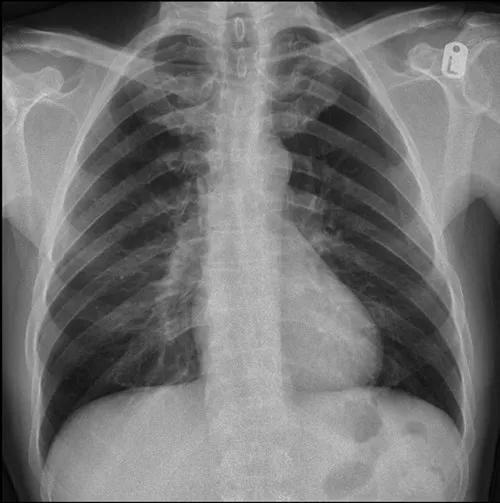
The radiologist report on this chest x-ray is "The heart is not enlarged. There is modest prominence of the pulmonary arteries bilaterally. The lungs are otherwise clear in this patient with an incidental azygous fissure.” It does not suggest PAH.
The chest x-ray is abnormal in 90% of people with Idiopathic Pulmonary Arterial Hypertension (IPAH) at the time of diagnosis. Typical changes include enlarged pulmonary arteries with peripheral pruning of vessels and cardiomegaly. There may be changes suggesting an alternative cause of PH such as lung disease or pulmonary venous congestion.
Case study summary
Listen to the expert summary on this case
Recommendation is for continued follow up with transthoracic echo, consequently the patient does not need referral to a specialist PH centre.